With nearly 20% of the adult U.S. population opting into a Medicare plan in 2024, and those numbers are anticipated to grow in the next decade, there is a need in the market for coverage options. Medicare plans that are working to proactively stay ahead of the competition by focusing on how to retain and attract customers will see powerful benefits reflected in their Star Rating.
Do You Have a Clear Path to Improve Star Ratings?
From 2023 to 2024, CMS shared that the average plan ratings saw a dip for the second year in a row – from 4.14 to 4.04, already down from 4.37 in 2022. We often hear from Medicare Advantage leaders, “We have initiatives to drive towards 4 Stars next year.”
Reaching a 4-Star threshold grants Medicare Advantage plans more benefits and reflects strong consumer satisfaction. However, it’s often a challenge for leaders to understand the reasons and drivers behind lower-than-expected Star performance in key categories.
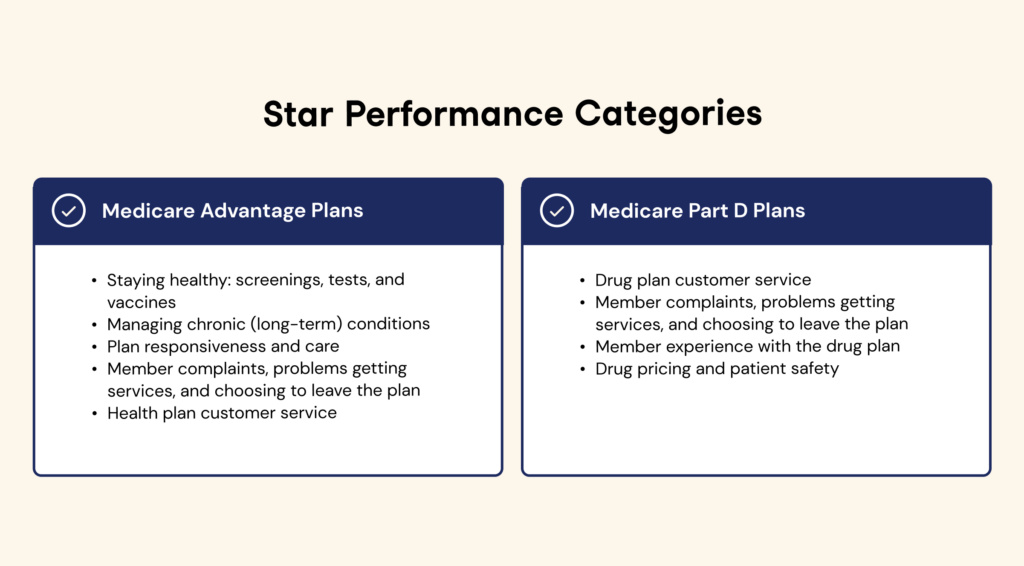
While Consumer Assessment and Systems (CAHPS) captures feedback annually, the results may lack context and only provide an annual read-out – two limiting factors in building a strategic plan to pivot and adjust in order to improve Star Ratings. Medicare Advantage leaders need a clear path to aggregate, review, and act on member experience data.
3 Ways AI is Being Used to Improve Star Ratings
Artificial intelligence (AI) is unlocking new ways to analyze data and aggregate insights, creating a path for Medicare Advantage leaders to improve and maintain Star Ratings. Specifically, member conversations hold valuable data that can lead to real revenue impact. Medicare-specific AI models uncover emerging trends and identify the biggest issues facing members, the brand, and employees.
Leveraging AI tools to listen directly to and strategically act on member feedback leads ways to improve Star Ratings.
- Leverage real-time feedback from members
- Observations without context can’t facilitate action. To understand why friction exists, organizations need to establish ways to gather and assess unsolicited feedback, quickly, reliably, and at scale. AI can analyze conversations and other unstructured data sources so member insights can be directly applied to business growth strategies. In the moment, AI helps Medicare leaders:
- Understand what members value and dislike about your plan
- Identify current friction points impacting enrollment and retention issues
- Find solutions for repeat callers before they decrease NPS and CSAT scores and sentiment (and increase costs)
- Observations without context can’t facilitate action. To understand why friction exists, organizations need to establish ways to gather and assess unsolicited feedback, quickly, reliably, and at scale. AI can analyze conversations and other unstructured data sources so member insights can be directly applied to business growth strategies. In the moment, AI helps Medicare leaders:
- Improve results with strategic prioritization
- Open enrollment is not the time to understand the member journey and learn there are friction points along the way. The marketplace is competitive, with different options and coverage plans among various providers. AI offers a competitive advantage in being able to strategically direct resources to best enhance and support the member experience, so plans are prepared well ahead of this year’s open enrollment period.
- Aggregate reports that highlight trends and improvement over time
- Pinpoint recurring issues, complaints, and barriers
- Quantify how your process is navigated with context
- Open enrollment is not the time to understand the member journey and learn there are friction points along the way. The marketplace is competitive, with different options and coverage plans among various providers. AI offers a competitive advantage in being able to strategically direct resources to best enhance and support the member experience, so plans are prepared well ahead of this year’s open enrollment period.
- Be proactive and get started
- This year’s Star Ratings are already reported. Are you where you want to be? Do you have a plan to maintain your current status? If the answer is no, AI can be a proactive measure to cut through the noise to understand what is valued most about the current plan and be invaluable in rising above your competitors. If yes, AI can help improve efficiencies in executing the plan and validating the team’s strategic direction.
- Adjust offerings prior to the next open enrollment
- Invest strategically to retain members and limit churn
- Detect complaints and grievances in real time to better ensure resolution
- This year’s Star Ratings are already reported. Are you where you want to be? Do you have a plan to maintain your current status? If the answer is no, AI can be a proactive measure to cut through the noise to understand what is valued most about the current plan and be invaluable in rising above your competitors. If yes, AI can help improve efficiencies in executing the plan and validating the team’s strategic direction.
An AI Solution to Improve Star Ratings
Authenticx was built intentionally with Medicare providers in mind to help improve quality and retention with an AI-powered solution.
Our platform uses proprietary AI models to give providers data-backed insights to drive strategic business decisions, member retention, and superior service experiences.
Learn more about our work with Medicare Advantage providers by reading this success story.

About Authenticx
Authenticx is the new standard for humanizing conversational intelligence in healthcare by analyzing millions of customer interactions (like voice, chat, or emails) to surface immersive and intelligent insights at scale. Authenticx was founded to aggregate, analyze and activate customer interaction data to surface transformational opportunities in healthcare. Using existing data that’s likely being stored and ignored in your organization, Authenticx reveals hidden barriers, motivators, and strategies so healthcare organizations can make confident, data-backed decisions. In 2023, Authenticx was ranked No. 349 on the Inc. 5000 recognized as one of America and Indiana’s fastest-growing private companies.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter/X | Instagram | YouTube