Authenticx for Insurance & Payers
Improve quality and retention with insights and automation.
Authenticx gives insurance providers the data to drive strategic business decisions, member retention, and superior service experiences with AI built for healthcare.
Stand apart from the competition
Understand leading drivers of dissatisfaction and churn to retain and grow.
Monthly Call Volume
3.5 Million
QA Evaluations – Scaled 4X with AI
Decrease Call Length
30 sec
Average reduction of call time company-wide in 3 months
Process Improvement
66%
Reduction of email backlog in 90 days
Positive member impact
Analyze member conversations at scale with AI to optimize service and agent performance.
AI Purpose-Built for Insurance
Built specifically for healthcare
AI models that are labelled and trained exclusively on healthcare data in-house.
Verticalized AI offers superior accuracy with better recognition of the terms, brand names, and process terminology.
Powerful insights fuel decision-making
Identify drivers of member attrition and friction to improve retention and experience.
Leverage member conversations to develop data-backed business plans that deliver results.
AI solutions for insurance & payors
Scale agent efficiency and evaluations of agent performance.
Diagnose source of member dissatisfaction to strategically invest resources.
Member Experience
Agent Performance
Process Efficiencies
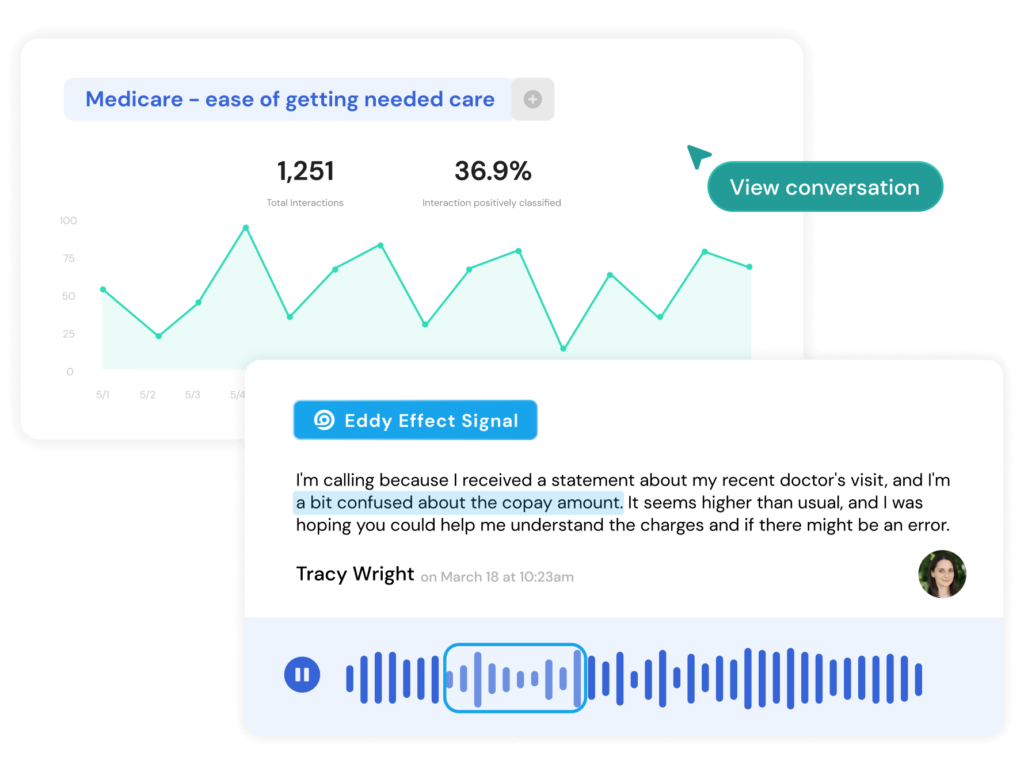
Uncover member feedback with AI to improve your Star rating
Understand what members value about your plan, what they dislike, and current friction points to attack enrollment and retention issues head on with proprietary AI models.

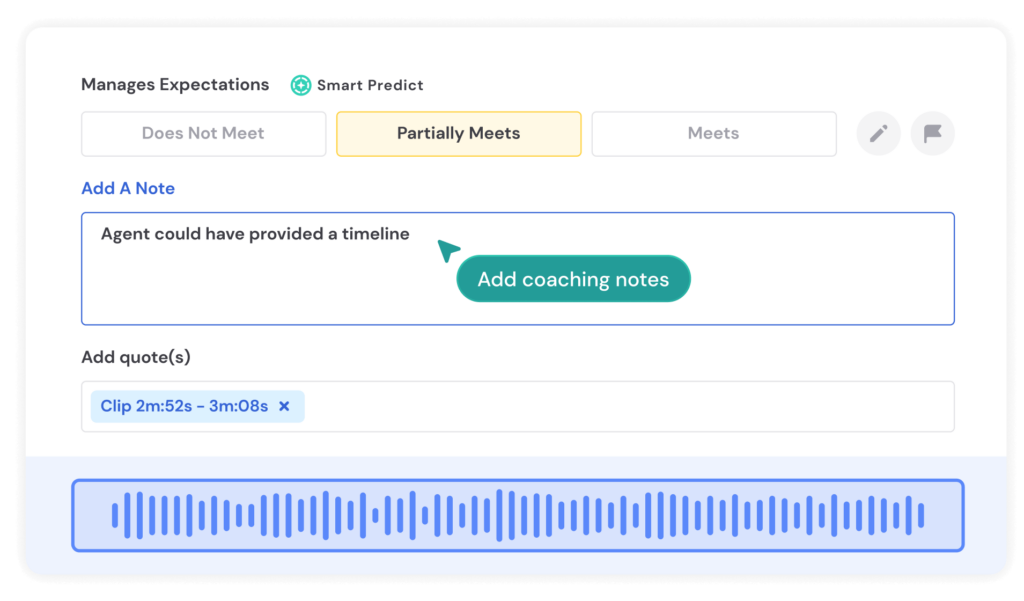
Scale QA evaluations with automation
Leverage AI tools to score agent performance, ensure compliance, and personalize manager coaching with individual assessments.
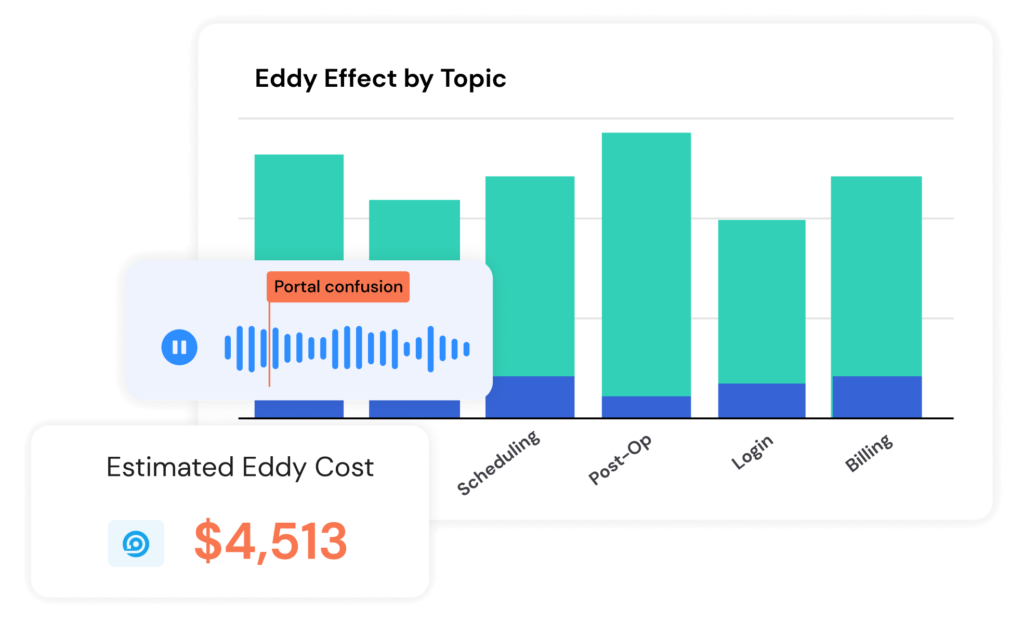
Identify drivers of broken process
Drill down into specific instances of customer friction to find operational inefficiencies and direct resources to a solution.
Medicare Providers
Prevent member churn with reliable, accurate insights. Drive strategic decision-making with conversation AI and data analysis.
- Quantify and contextualize how patients and providers navigate your process to best anticipate a positive Medicare star rating.
- Identify and address leading drivers of member attrition year over year.
- Gain valuable context on why patients stop or change coverage plans to address brand detractors ahead of open enrollment.