
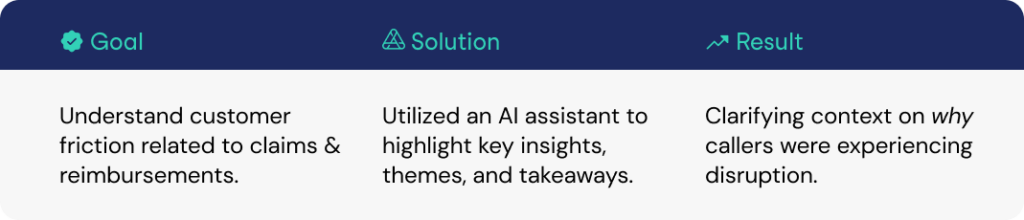
A pharmaceutical company used the Authenticx Insights Solution to leverage our AI assistant to investigate conversation themes related to claims and reimbursements. These topics were flagged as the primary driver of customer friction with an Eddy Effect rate of 34%.

Authenticx in Action
The AI assistant KBo highlighted key insights and takeaways with specific conversations as to why callers were experiencing disruption related to claims and reimbursements:
- Transcripts mentioned delays in claims processing which was leading to frequent follow-up communications
- There was caller confusion related to insurance coverage and billing, specifically on types of payment methods
- Unclear assistance and next steps with callers expressed uncertainty of their status or why they were waiting for a callback
- Customers struggled to understand insurance policies, specificially related to patient support programs and savings accounts
Results
The AI assistant KBo was able to analyze call transcripts at scale, which revealed recurring themes of customer frustration. Communication breakdowns between agents and callers were also complicating issue resolution.
With these insights, the team is leveraging the KBo as a guide to improve training and seek opportunities to streamline systems for more efficient service delivery to their healthcare providers (HCPs).

About Authenticx
Authenticx was founded to analyze and activate customer interaction data at scale. Why? We wanted to reveal transformational opportunities in healthcare. We are on a mission to help humans understand humans. With a combined 100+ years of leadership experience in pharma, payer, and healthcare organizations, we know first-hand the challenges and opportunities that our clients face because we’ve been in your shoes.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter | Instagram | YouTube