
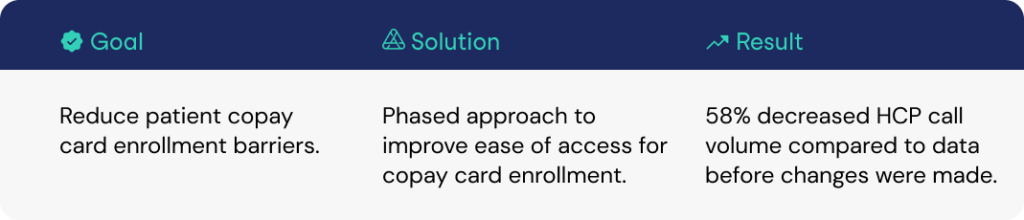
A pharmaceutical company leveraged the Authenticx Quality Solution to analyze their implemented patient copay card enrollment process improvements in order to monitor if they had a positive impact. The team was tasked to reduce current enrollment barriers for patients and healthcare providers (HCPs).
Authenticx in Action
Using conversation data to derive AI-driven insights, Authenticx helped the pharmaceutical company improve their enrollment experience. This resulted in a phased approach. Phase 1 helped reduce the time the copay card was received by five days (from about a week to a single day). Phase 2 gave instant access for patients receiving a copay card.
Results
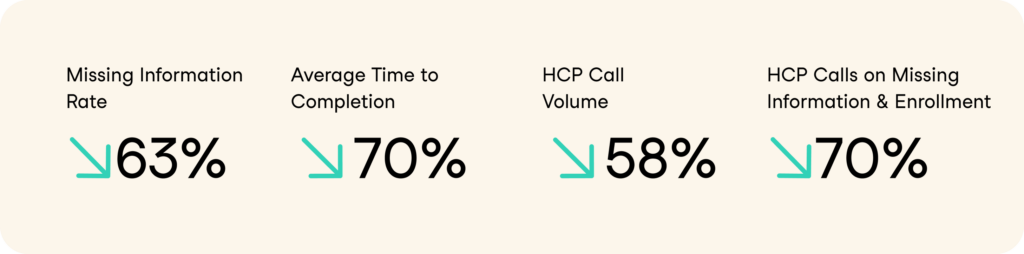
To measure success, the team compared data before changes were made to after the changes were implemented. From this two-phase approach, the team reported the following results due to AI-driven insights:
- Missing Information rate decreased by 20%
- Average time from enrollment to copay case completion decreased by 70%
- HCP call volume decreased by 58%
- HCP calls about Missing Information and Enrollment Forms decreased by 70%
Having clear insight into how process improvements are in place is an important component in building a positive, impactful patient and HCP experience.
About Authenticx
Authenticx was founded to analyze and activate customer interaction data at scale. Why? We wanted to reveal transformational opportunities in healthcare. We are on a mission to help humans understand humans. With a combined 100+ years of leadership experience in pharma, payer, and healthcare organizations, we know first-hand the challenges and opportunities that our clients face because we’ve been in your shoes.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter | Instagram | YouTube