
As previously shared in the first part of our Crushing Complexity blog series, the size and scope of the healthcare industry is immense, which exists in a complex interconnected burden for patients to manage both their care and the business of their care.
Based on the analysis of 200 million recorded conversations between patients and their providers, payers, and pharmaceutical companies, this 3-part series is exploring the current United States healthcare system, as reflected in the voices of customers, and emerging innovations that can be leveraged to ease the burden for millions of patients and caregivers. Healthcare impacts all of us, and it will take a coordinated and collaborative effort to enact change.
Globally, the United States outspends other high-income countries on healthcare, but achieves poorer results on important measures of healthcare outcomes, according to the Commonwealth Fund Global Perspective report.
But in order to consider how we might improve our ranking, we must first consider how our healthcare system has evolved, both in terms of the care we provide and the way we pay for it.

A Historical Lookback on the Business of Healthcare
The system we know today has come a long way from the early days of healthcare in our country. Just two centuries ago, traditional care would have come from house doctor visits — if the patient was of a particular social class and race and lived in a town with a doctor in residence. While care was approached case-by-case, there was limited knowledge and few effective treatment options to address symptoms.
Hospital Systems and Medical Standardization
In the 1860s, public hospitals, or centralized places for care, began to emerge. Initially run by charities, as medical practices evolved and populations grew, hospital administrators gradually developed a business mindset that altered the administration of care. So too, as clinical practices evolved, the practitioners of medicine needed standardization within the discipline, which altered the status of the profession. By 1898, all states had medical licensing boards and medical schools had adopted a standard curriculum.
Insurance Standardization and Rapid Expansion
The popularity of new, not-for-profit health insurance offerings in the 1930s expanded in the post-Depression era. World War II then ignited further growth of insurance as an incentive to attract workers as growing numbers of men were drafted into service. This era linked health insurance as a labor benefit for employers and employees to use as a bargaining tool for talent competition. In fact, prior to World War II, approximately just 9 percent of the population had some form of health coverage; after the war, that jumped to 23 percent. By 1960 up to 70 percent of the population had employee-based commercial insurance coverage. To finance the care of the unemployed, federally-sponsored healthcare, in the form of Medicare, was passed by Congress in 1965 with Medicaid expansion throughout the 1980s.
Medical Regulations and Medicine Specialization
The last 40 years of healthcare innovation have ushered in medical advancements at an exponential rate, in part due to specialization of diagnostics and treatment, leading to new therapies and enhanced drugs. But these advancements have come with rising costs The CMS reported retail prescription drug spending increased 7.8 percent to $378.0 billion in 2021 (compared to an increase of 3.7 percent in 2020).
Medical advancements have also led to the expansion of government regulations and ever-evolving insurance coverage options like HMOs, PPOs, consumer-directed health plans, and the Affordable Care Act. The CMS reported retail prescription drug spending increased 7.8 percent to $378.0 billion in 2021 (compared to an increase of 3.7 percent in 2020).
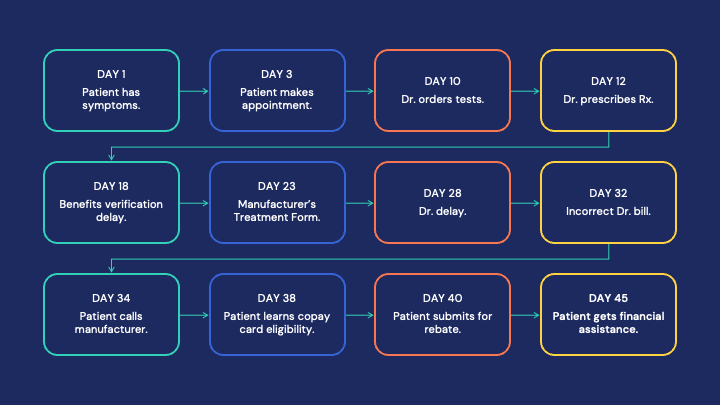
This history demonstrates the remarkable ingenuity, expansion and progress the industry has made to provide coverage and high quality care. However, we cannot ignore the fact that alongside this progress has inadvertently come a crushingly complex and fractured system. Healthcare started as a one-on-one experience but now patients are consumed by massive healthcare entities: healthcare providers, insurance organizations, pharmacies, government groups, professional caregivers, and medical manufacturers. As the business of healthcare has evolved to accommodate its clinical advancements, the consumer has gotten caught in the middle of powerful organizations with often competing goals. This evolution results in more steps along the patient journey, which increases time and can, ultimately, impact care.
3 Takeaways for the Future Business of Healthcare
We can’t discount the progress that has been made through human ingenuity to drive change and innovation to improve health outcomes and control costs. But the complex system that has emerged poses abundant opportunities for improvement. Three such opportunities include the following:
Social Determinants of Health and the Business of Healthcare: Recent progress has been made to expand access to healthcare by understanding Social Determinants of Health. By also understanding the experience of at-risk patients in navigating the complex language and business of healthcare, we can learn what is needed to simplify processes and business navigation for patients and caregivers.
See it in Action: Read this story to see how a hospital system used AI to better understand social barriers preventing patients from attending their appointments
Resource Development and Education: To understand what specific education and information would ease the burden of patients and caregivers in managing the business of their healthcare, we can listen at scale to what they’re telling us in naturally occurring conversations. The depth of understanding that comes from listening can offer direction on how leaders can make decisions that provide more positive customer experiences. Listening at scale gives leaders context and depth of insight around what information and education their customers need.
See it in action: Read this story to see how a biopharmaceutical company was able to listen to customer stories to understand the root of their confusion and, in turn, create training resources for employees to better address patient concerns.
Operational Process Impact: Better understanding the root causes of patient obstacles can ultimately drive operational changes that improve patient experiences and health outcomes. Organizational processes, such as employee coaching and training, process improvements, data analysis, and resource messaging all play a role in the patient experience. Examining how operational processes can ease the burden for patients and caregivers managing the business of their healthcare is critical for both patient health outcomes and company business outcomes.
See it in action: Read this story to see how a life sciences manufacturer used conversations to improve internal processes to increase therapy adherence and improve the patient journey.
Our past informs the future. Healthcare, as well as the business of healthcare, has experienced immense evolution in the past century. As the industry continues to step forward with new tools, insights, and approaches, we must recognize the positive and negative impact being felt to align on what’s next.
Continue to Part 3 here: What’s Next? Start Listening with Conversational AI Tools for Healthcare
Authenticx + Crushing Complexity
Healthcare impacts all of us; this story is OUR story. Authenticx is excited to introduce Crushing Complexity: The Evolving Business of Healthcare, created by Sally Perkins. This presentation is a conversation starter around the business of healthcare, examining the past and present to prompt action for a more hopeful future. No one can deny the fact that healthcare in the U.S. is complex. But how did we get here? How do patients and caregivers experience that complexity? And are we, in fact, crushing it, or is it crushing us? Based on the study of millions of conversations from all segments of healthcare— payers, providers, and pharmaceuticals— this presentation takes a 30,000-foot view of our healthcare system and its impact on consumers and business outcomes.
Audiences come along on a journey through time, and into the experiences of patients and caregivers, to confront the complexity of the U.S. healthcare system and inspire us all to take a hard look at what we’ve created and why it must change.
We believe the key to enacting change is to listen to patients, putting their voices in the center of healthcare business discussions.
ABOUT SALLY PERKINS
Sally Perkins serves as an Insight Storyteller at Authenticx, a conversational intelligence company. In her role as an Insight Storyteller, Sally analyzes quantitative and qualitative conversational data from which she crafts impactful data-backed stories that offer insights into how healthcare organizations can improve the customer experience and improve business outcomes.
Prior to her work at Authenticx, Sally was a Professor of Rhetorical Studies at California State University Sacramento and an adjunct faculty member at Butler University in Indianapolis. She is also a professional story performer and has trained hundreds of professionals on telling compelling stories to accomplish business objectives. On Sally’s best days, she can be found telling stories to kids at Riley’s Hospital for Children in Indianapolis.
About Authenticx
Authenticx was founded to analyze and activate customer interaction data at scale. Why? We wanted to reveal transformational opportunities in healthcare. We are on a mission to help humans understand humans. With a combined 100+ years of leadership experience in pharma, payer, and healthcare organizations, we know first-hand the challenges and opportunities that our clients face because we’ve been in your shoes.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter | Instagram | YouTube


