
Due to new guidance from the California Department of Managed Health Care, a top-ten nationwide health insurer was required to increase their monitoring for appeals and grievances from 1.5% to 5% of all calls within six months.
By scaling these compliance monitoring efforts with Authenticx, the organization sought to meet this new requirement ahead of deadline and without increasing headcount or incurring added costs.
Authenticx in Action
By leveraging Authenticx AI-completed evaluations and SmartPredict™ technology, the organization created unprecedented efficiency, unburdening human analysts from high-volume routine monitoring to instead focus on specific calls containing intricate processes, high-risk interactions, or critical errors.
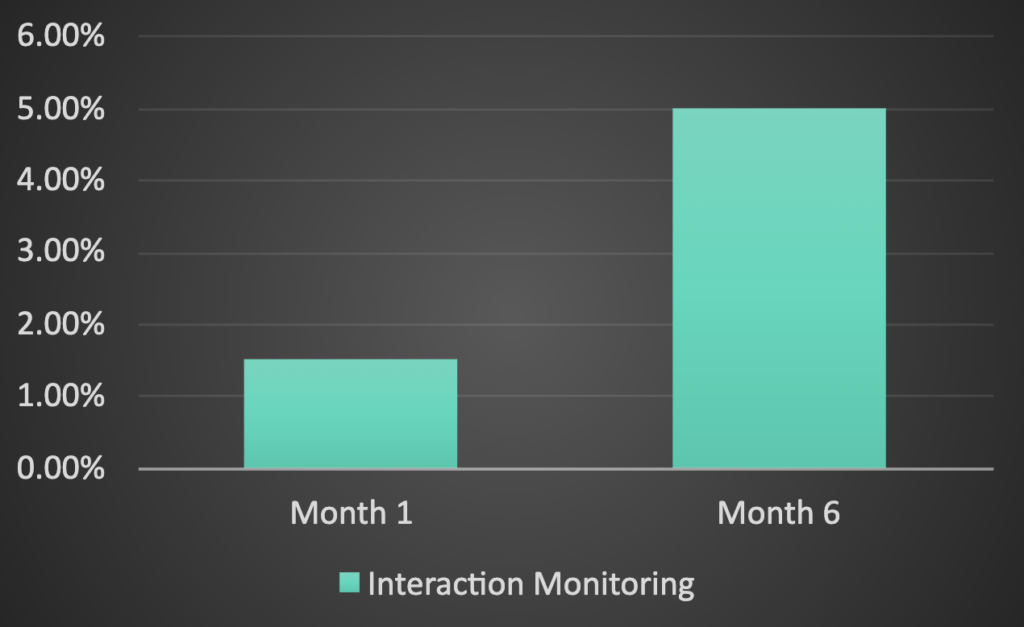
Results
At the time of the new regulations taking effect, the organization:
- Met all regulatory requirements ahead of deadline
- Incurred no new cost (beyond existing Authenticx partnership) while significantly scaling compliance monitoring
- Mitigated its risk of future complaints and audit findings
See Authenticx in Action
Learn more about how Authenticx analyzes customer conversations to surface recurring trends in this two-minute video.
About Authenticx
Authenticx was founded to analyze and activate customer interaction data at scale. Why? We wanted to reveal transformational opportunities in healthcare. We are on a mission to help humans understand humans. With a combined 100+ years of leadership experience in pharma, payer, and healthcare organizations, we know first-hand the challenges and opportunities that our clients face because we’ve been in your shoes.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter | Instagram | YouTube


