
Elevating CAHPS Scores & Medicare Star Ratings
Objectives
A highly-competitive, top-5 Medicare health plan used Authenticx to elevate CAHPS scores and Star Ratings by using member insights to uncover and reduce friction points, or Eddies, that impact the member experience. To do so, we collaboratively implemented the following objectives:
- Leverage full-volume conversational insights in the Authenticx platform
- Uncover member confusion and barriers
- Conduct a comprehensive process review
- Activate insights to drive positive CAHPS/Star Ratings outcomes
Authenticx in Action
Authenticx proprietary AI models were tuned to focus on specific topics in recorded member conversations indicating negative member experiences; these friction points could correlate with less-than-favorable CAHPS scores and resulting Star Ratings.
Following this initial period of listening at scale, the team identified a member-wide Eddy Effect rate of 22%, meaning that members were experiencing disruptive friction in nearly a quarter of all calls.
After quantifying prevalence, the team used the Authenticx Insights Module to identify not only the top drivers of member friction, but also how it was impacting care and plan satisfaction. They discovered that:
- A large majority of Eddies (over 70%) were caused by either processes or technology
- In nearly 1/3 of these Eddies, members experienced delayed treatment, and almost 20% of Eddies negatively impacted members financially
- The plan’s online member portal was a specific source of friction. Members were having difficulty navigating the portal to enroll in, interact with, or cancel their plan
Results
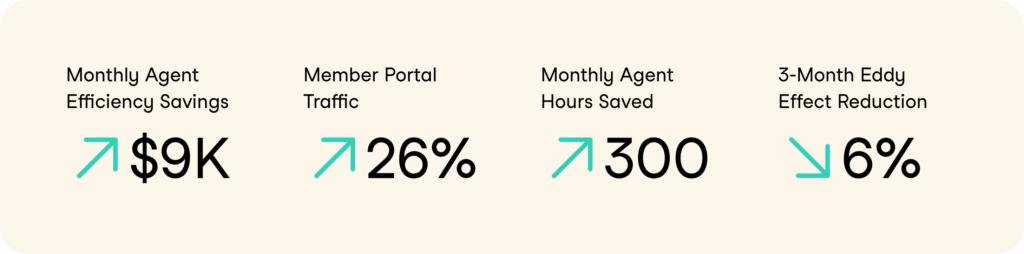
Armed with actionable insights from Authenticx, the organization re-aligned processes and resources to elevate the member experience. They re-prioritized internal tech resources to urgently address the website portal, redesigning the site’s UX and navigability with simplicity in mind. Next, they updated agent training scripts and guides to better clarify the portal process. These changes resulted in a 26% increase in member portal site traffic and over 300 hours per month saved in agents’ time formerly spent addressing portal issues.
As a whole, surfacing and addressing member-facing Eddies led to:
- Tangible savings in reduced call volume (more service could be provided via the portal)
- Nearly $10,000 per month saved in agent efficiency (members were getting stuck in fewer complex problems)
- A 6% overall reduction of caller friction within just three months
Why It Matters
For Medicare payer organizations, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey is a vital tool used to measure the experiences of members with their Medicare plans and healthcare providers. Managed by the federal government’s Centers for Medicare & Medicaid Services (CMS), this annual CAHPS survey collects feedback on members’ experiences ranging from communication and provider coverage to health outcomes, satisfaction, and more.
For CX leaders at Medicare payer organizations, the insights from the CAHPS survey are crucial: they help assess and improve the quality of plans, pinpoint opportunity areas, and align services with the changing needs of their members.
Concurrently, Medicare Star Ratings are a specific outcome of CAHPS survey results. These ratings, ranging from one to five stars, serve as a performance benchmark for Medicare Advantage and Prescription Drug Plans, evaluating criteria such as clinical outcomes and member experience from CAHPS survey responses and other sources. For payer organizations, achieving high Star Ratings is not just a brand attractor — it’s a strategic necessity. Higher ratings not only indicate member satisfaction and plan health; they also directly impact the financial incentives that payer organizations receive from the federal government.
Together with the CAHPS survey, Star Ratings are an essential tool for payer organizations to measure performance, drive improvement, and provide excellent service to their members.
By the Numbers
—
Quality Excellence Through Listening at Scale
Objectives
A leading Fortune-500 payer organization used Authenticx to scale their quality program using AI. In order to handle the nearly 3.5 million member interactions their contact centers receive per month (primarily in the form of phone calls and online chats), the insurer’s quality leaders oversee a team of over 10,000 member-facing agents and nearly 200 dedicated quality analysts. But despite this massive volume of conversations, the team performed manual QA audits on less than 1% of these interactions before using Authenticx — presenting a prime opportunity to use technology at scale.
Authenticx in Action
Authenticx worked with the insurer’s quality team, technical leaders, and telephony partners to quickly and efficiently implement AI-completed evaluations and the Authenticx agent coaching solution across the organization.
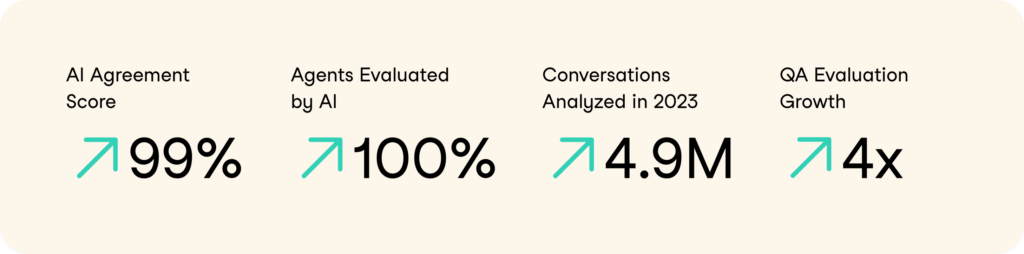
In order to train the AI models specifically to the insurer’s quality criteria, the teams leveraged standardized “AI Agreement” metrics that human analysts cross-referenced AI results against. Beginning with an initial baseline Agreement Score of 69% (i.e., the AI evaluations matched the human evaluations 69% of the time), they made regular enhancements to further train the software — and within months, they achieved an overall consistent agreement score of 99% across all calls.
With this solution in place, Authenticx AI accurately and efficiently analyzed nearly 4.9 million of the organization’s conversations in 2023: QA was now being performed at scale.
Results
In just five months, the organization successfully expanded its agent-specific QA initiatives by 30%, covering the assessment of 100% of agents across the enterprise. And within ten months, the total number of evaluations grew by over 400%, resulting in substantial savings in headcount costs through the efficient use of technology. Leveraging Authenticx, the team not only evaluated more than 150,000 calls each month but also established a benchmark for organizational quality based on this AI-informed evaluation data.
Additionally, the implementation of Authenticx’s agent coaching solution facilitated real-time, bi-directional feedback between analysts and agents. This enhanced level of transparency and confidence proved crucial for employee retention and laid the foundation for a reimagined quality program within the organization.
Why It Matters
For enterprise payers, analyzing a subset of member calls is a standard practice to monitor and improve agent quality outcomes. But by augmenting these efforts with cutting-edge AI models like natural language understanding (NLU), large language learning (LLMs), and sentiment analysis, quality leaders at health insurance organizations can efficiently capture and learn from the entire enterprise universe of member conversations — not just a small sample. This automated approach forms the foundation of what we refer to as listening at scale.
By listening at scale, contact center and QA leaders can be more proactive at enhancing agent performance. They can quickly and holistically recognize successful communication strategies and skills used by agents and highlight areas for improvement, allowing for targeted training and support. By automating the process of call analysis at scale, QA and CX leaders can streamline performance management, gain real-time insights, and ultimately drive improvements in member satisfaction. AI-powered tools not only optimize operational efficiency but also provide a strategic advantage in delivering high-quality customer service, ensuring that member relationships are built on a foundation of high-quality, responsive, and informed interactions.
By the Numbers
—

About Authenticx
Authenticx was founded to analyze and activate customer interaction data at scale. Why? We wanted to reveal transformational opportunities in healthcare. We are on a mission to help humans understand humans. With a combined 100+ years of leadership experience in pharma, payer, and healthcare organizations, we know first-hand the challenges and opportunities that our clients face because we’ve been in your shoes.
Want to learn more? Contact us!
Or connect with us on social! LinkedIn | Facebook | Twitter | Instagram | YouTube


